Oxygen Concentrators

Inogen® provides oxygen concentrator solutions for both portable and stationary use.
Our Inogen® portable oxygen concentrators were developed to be small, light, and quiet for use at home or while traveling. This innovative product family has been thoughtfully designed for patients seeking lightweight devices such as a portable oxygen concentrator. With two models available for purchase — the Inogen® Rove 4™ and Inogen® Rove 6™ — Inogen® portable concentrators provide supplemental oxygen “on-the-go”1.
For stationary oxygen therapy, the Inogen At Home® provides continuous flow oxygen up to 5 liters per minute in a small, compact and light design. Learn more about the Inogen At Home® below. The NEW Inogen® Voxi™ 5, starting at $795, provides a valuable option for a stationary oxygen concentrator. Learn more about Inogen’s stationary solutions below.

“When I was on tanks, I felt imprisoned. Now that I’ve got my Inogen One, my life is full again. With this little device, I can go anywhere and do the things I love.”§
— Len B.

Finally, oxygen delivery reimagined. No tanks required! Our lightweight, easy-to-use stationary and portable oxygen concentrators help you move about your home—and out and about in the world!

"I was born on the 4th of July so freedom is a big deal! So to be tethered to an oxygen machine was not my favorite thing. But the Inogen One is very easy to operate and you barely notice it's there.Ӥ
— Claudia H.
Three Oxygen Concentrators to Choose From

Rove 4™ System
- 2.9 lbs with standard battery
- 4 pulse-dose settings
- 3 battery configurations for versatility
- Inogen's reliable pulse-dose based Intelligent Delivery Technology®
- Meets FAA acceptance criteria for carriage and use on board aircraft
The Inogen® Rove 4™ delivers power and performance in a compact POC, giving you the lightest weight and highest oxygen output 4-setting POC available today2. With three battery options, you can feel confident to continue normal activities of daily living. Designed for reliability, the Inogen® Rove 4™ offers best in class expected service life of up to 8 years3.
Inogen® Rove 4™ Systems
Rove 6™ System
- 4.8 lbs with standard battery
- 6 pulse-dose settings
- 2 battery configurations for versatility
- Inogen's reliable pulse-dose based Intelligent Delivery Technology®
- Meets FAA acceptance criteria for carriage and use on board aircraft
The Inogen® Rove 6™ offers a solution for patients looking for an oxygen delivery system that is quiet4 and compact. The Inogen® Rove 6™ provides an adaptable design as a lightweight device that has multiple product configurations for life on the go. Patients can feel peace of mind to take time to roam – like spending quality time with family and friends, enjoying the great outdoors, and traveling.
Inogen® Rove 6™ Systems
Inogen At Home System
- 1-5 liters per minute, continuous flow
- 18 pounds
- Quiet
- Energy-efficient, 100W on Setting 2
Our Inogen At Home® system combines up to 5-liter per minute continuous flow oxygen delivery with technology that is quiet, letting you watch TV or visit with friends with little noise disturbance.
At just 18 pounds, Inogen At Home® is a compact unit you can keep at your bedside or use it during the day as a companion around the house. The Inogen At Home® is energy efficient to help you save on electric costs over time.
Inogen At Home® System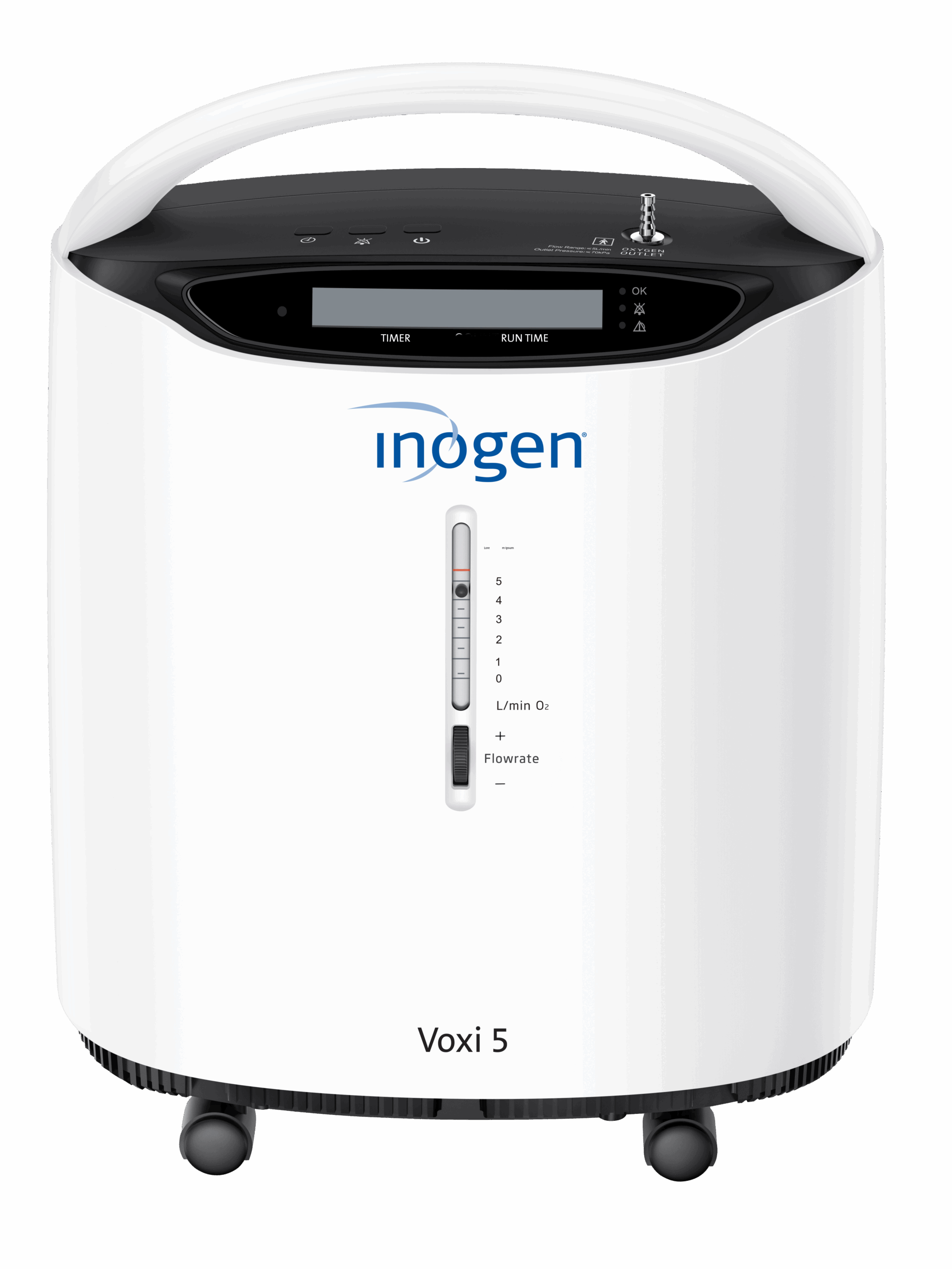
Voxi™ 5 System
- 1-5 liters per minute continuous flow
- 34 lbs on caster wheels
- Compact and quiet, at typical flow setting
The Inogen® Voxi™ 5 is a compact and durable stationary oxygen concentrator solution. Whether around the house or at your bedside, the Inogen® Voxi™ 5 can be your stationary solution to at-home oxygen therapy.
Inogen® Voxi™ 5 SystemWhy Choose an Inogen® Oxygen Concentrator?
Inogen® portable oxygen concentrators give patients peace of mind when outside their home and away from their stationary concentrator. Our portable oxygen concentrators are designed for the travel needs of our active patients and their lifestyle.
If your doctor recommends supplemental oxygen, we have a number of Inogen® products and equipment designed for your on-the-go lifestyle. Find out more about how our portable oxygen concentrators can provide your prescribed oxygen at home or away, all day, every day. Contact us today for help from our experts.

Inogen Connect The Bluetooth App
Introducing Inogen Connect, the free mobile app now available for Inogen devices. Monitor your Inogen concentrator with your phone to check battery life and column status, set maintenance reminders, receive special discounts and more. Download the app for free from the Apple App Store or the Google Play App Store.


2 2.9 lbs when used with standard battery delivering up to 840 mL/min of medical-grade oxygen. Tested against current POCs available on the market. Data on file and available upon request.
3 When used for less than 8 hours per day
4 37 dBA on flow setting 1